There’s a meme currently going around that’s a video of a wildly skilled swordswoman trying to strike another woman. The problem? Her opponent’s reflexes are unmatchable. Each time the sword nears her, she dodges out of the way with cat-like instinct. The accompanying caption? People who still haven’t got COVID.
To say the omicron variant is pervasive is an understatement (though, fortunately, kids are still far less likely to become severely ill). And because of this — and because kids under 5 still aren’t eligible for vaccination — it may feel like every family around you is popping up with a positive case while you and your family, like the swordswoman, try to duck and dodge and tumble away from its strike.
“While we have a lot more to learn about the trajectory of COVID, as time goes on, we hope the number of infections and hospitalizations and deaths will be less than prior with improving vaccination and booster rates,” notes Dr. Larry Kociolek, attending physician in the division of infectious diseases and medical director of infection prevention and control at Lurie Children’s Hospital in Chicago. “We can also minimize intermittent bumps in activity by masking and avoiding contact with others when sick.”
“While we have a lot more to learn about the trajectory of COVID, as time goes on, we hope the number of infections and hospitalizations and deaths will be less than prior with improving vaccination and booster rates.”
— DR. LARRY KOCIOLEK, PHYSICIAN
But even with brighter futures (hopefully) on the horizon, the recent surge is leading parents to question how to proceed through a variety of scenarios. What if your child has symptoms, has a close-contact exposure to someone with COVID or, ultimately, tests positive for COVID? Read on for the expert protocol.
What, generally, are the symptoms of COVID in kids?
Cold, flu, COVID? Who knows these days, as so many symptoms overlap — and with COVID, the symptoms are wide-ranging in kids. That said, here are the most common COVID symptoms in kids, according to Dr. Jessica Hommel, a pediatrician from Holston Medical Group in Bristol, Tennessee, and Dr. Jennifer Kusma, a pediatrician with Ann and Robert Lurie Children’s Hospital of Chicago and Instructor of Pediatrics at Northwestern University — but keep in mind, some kids will only have some (or even just one) of these:
- Fever.
- Cough.
- Runny nose.
- Congestion.
- Sore throat.
- Headache.
- Body aches (more common in teens).
- Dizziness (more common in teens).
- Gastrointestinal symptoms, such as nausea, vomiting and diarrhea (more common in teens).
What is the protocol for kids with symptoms?
1. Head to the doctor if symptoms are severe
First and foremost, Kusma says that if your child has any of the following symptoms (which may or may not be COVID), head to the doctor:
- A temperature greater than 100.4 F for more than three days.
- A fever in a child under 2.
- Difficulty breathing.
- Inability to drink and stay hydrated.
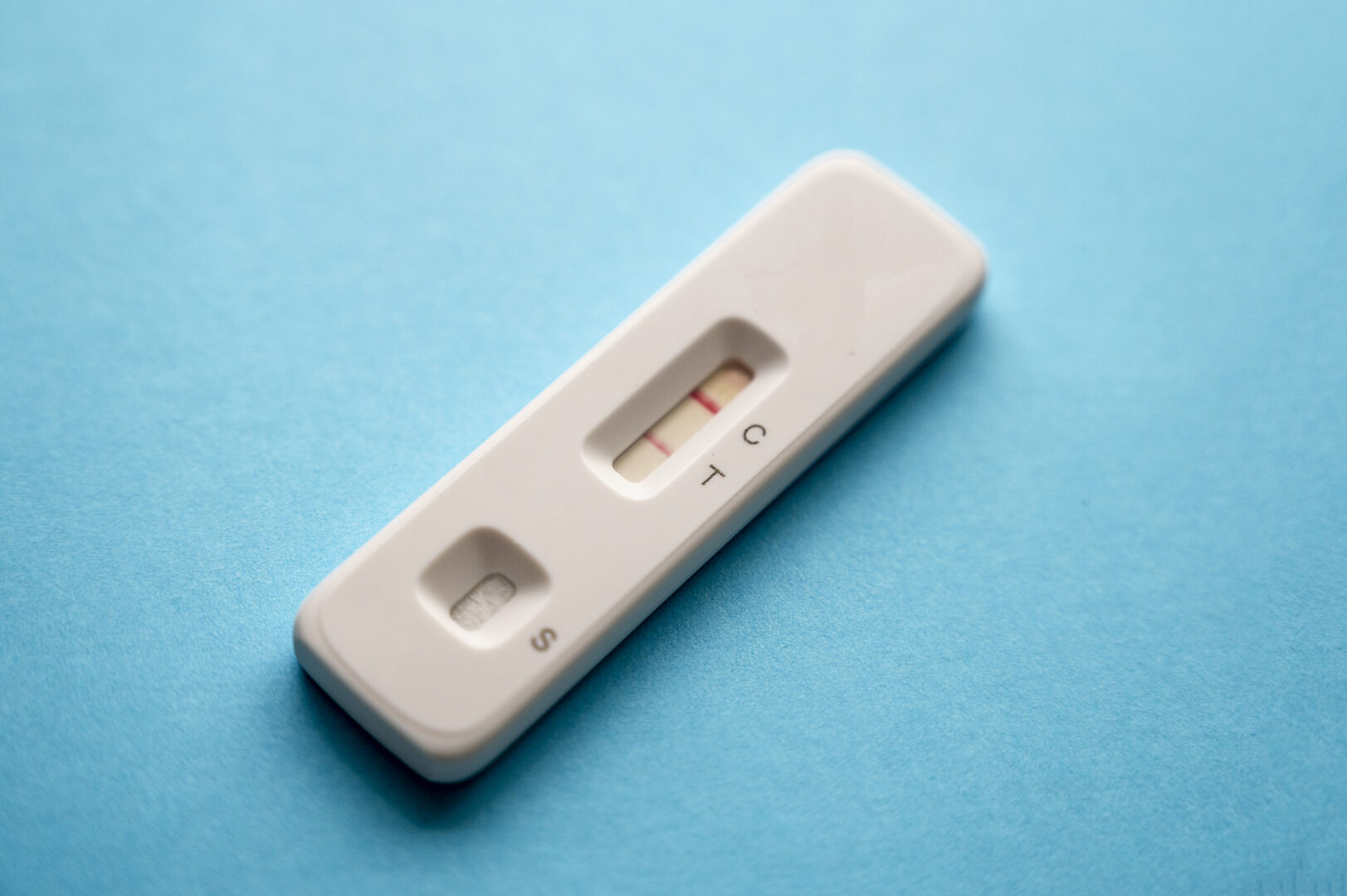
2. Rule out COVID by testing:
It’s hard to believe, but non-COVID viruses do still exist. However, it’s important to know whether or not the symptoms your child is presenting with are indeed COVID, as different protocols will apply if it is.
“Generally speaking, if your child is exhibiting symptoms that could be consistent with COVID-19, such as a new onset cough, fever, congestion, nausea, vomiting or body chills, you should have them tested,” says Kusma. “However, you don’t have to go straight to your doctor to do this.”
While a number of places, such as drugstores and community-based testing centers, offer COVID testing, the latest omicron surge has created a testing shortage, making it difficult to nab a polymerase chain reaction (PCR) test appointment. At-home antigen tests, also known as rapid tests, are also very limited.
If you can’t get a test for your child, but suspect they may have COVID — you guessed it — keep them home. (More on this shortly.)
3. Don’t test too early
Instead of heading to the pediatrician for testing the moment your child sneezes, Hommel recommends waiting it out a bit to allow symptoms to fully develop.
“If your child is experiencing non-emergency symptoms, such as a cough or runny nose, monitor their symptoms for at least 24 hours before visiting a provider for COVID-19 testing and/or care,” says Hommel. “This allows symptoms to fully show within a child and prevent early testing, which often results in a false negative.”
“If your child is experiencing non-emergency symptoms, such as a cough or runny nose, monitor their symptoms for at least 24 hours before visiting a provider for COVID-19 testing and/or care.”
— DR. JESSICA HOMMEL, PEDIATRICIAN
Kusma agrees. “The best time to test them is when they are symptomatic,” she says.
“The best time to test them is when they are symptomatic.”
— DR. JENNIFER KUSMA, PEDIATRICIAN
4. Consider an at-home test first, especially for older kids
If your child’s symptoms are consistent with COVID, and they’re overall doing well, Kusma says, you can pursue testing options, such as “community testing sites or at-home tests” (if you can find them).
“At-home antigen tests can be a great first line of testing,” Kusma says. “And if the test is positive, your pediatrician can recommend confirmatory testing if necessary.”
“At-home antigen tests can be a great first line of testing. And if the test is positive, your pediatrician can recommend confirmatory testing if necessary.”
— DR. JENNIFER KUSMA
Parents can administer an at-home test on their children, but for more accuracy, particularly when it comes to little kids, you should still head to the doctor or a community testing site that offers PCR tests.
“We often recommend coming in when a test is needed,” Hommel says. “Parents can do an at-home test, but with small children it can be hard to do correctly. And even for kids 12 or older, we still recommend an in-person test because they’re often more accurate than the at-home options.”
5. Follow up with your doctor if the at-home test is positive
If you have a positive, at-home test for your child, Kusma recommends reaching out to your child’s pediatrician to determine the next steps. “In some cases, we will recommend that it is not necessary to seek a PCR confirmatory test,” she says. “However, some schools will require a PCR test for return to school, and it may be in this case you are directed to a testing site as opposed to going to the doctor.”
What’s the protocol for kids who were exposed to COVID but have no symptoms?
If your child was exposed to someone with COVID — they were within six feet, for 15 total minutes, over a 24-hour period with someone who was infected with COVID — Hommel recommends testing “three to five days after exposure.” She explains that “this is likely when a patient will be experiencing the peak of their COVID symptoms.”
Timing around testing, in this case, also depends on your child’s vaccination status. According to Kusma, here’s when vaccinated and unvaccinated kids should test:
- Fully vaccinated kids. You can test five days after exposure or sooner if they develop symptoms. If they are negative, then they are considered to have not gotten COVID from that exposure.
- Kids who aren’t fully vaccinated. Test immediately on learning of exposure, and if the test is negative, test again five to seven days after exposure. You can test sooner than five days if your child develops symptoms.
“If you are confused about whether your child was exposed,” Kusma says, “speak with your pediatrician.”
Kusma also adds that for both unvaccinated and vaccinated children, wearing a well-fitting mask around others is recommended for “10 days after an exposure.”
What’s the protocol if we can’t find testing?
COVID tests in 2022 are what toilet paper was in the first half of 2020 — a hot and elusive commodity. The unfortunate paradox, of course, is that “no test” doesn’t mean “no COVID.”
“If your child cannot get tested because you do not have access to a test, but you have reason to suspect that they have COVID, such as they have been exposed or they have symptoms consistent with COVID, then the best thing you can do is have them quarantine at home for five days,” Kusma says. “After that, they can go out of the home in a well-fitting mask for five days if the child is no longer experiencing symptoms.”
“If your child cannot get tested because you do not have access to a test, but you have reason to suspect that they have COVID, such as they have been exposed or they have symptoms consistent with COVID, then the best thing you can do is have them quarantine at home for five days.”
— DR. JENNIFER KUSMA
How should parents care for kids with COVID?
Both Hommel and Kusma say that one of the most important things to do if your child has COVID is make sure they rest and stay hydrated. “Depending on your child’s symptoms, make sure your child is staying hydrated by offering frequent small volumes to drink,” Kusma says.
Other than that, they recommend treating the symptoms to help kids feel more comfortable. “This would include Tylenol or ibuprofen, or cold medicine if your child is old enough,” Hommel says.
“At this time, COVID-specific treatments are not approved for children under 12,” Hommel adds. “For those 12 and older, there are monoclonal antibody options for those considered high risk. I recommend parents speak to their pediatrician to discuss if that option is right for their child.
When is it time to call the doctor?
Both medical experts recommend calling your child’s doctor for kids who are exhibiting any of the following:
- A fever (a temperature greater than 100.4 F) for more than two to three days.
- Shortness of breath
- Worsening cough.
- Chest pain.
- Inability to drink or stay hydrated.
If symptoms are “severe or life threatening,” Hommel recommends going to the emergency room.
Additionally, she advises parents to monitor their child’s temperature the following four to six weeks after a positive test. “A spike in temperature is one of the first symptoms of MIS-C and can lead to inflammation of other organs,” Hommel says. “As a parent, you know your child’s recovery time, and if you feel uncomfortable or don’t feel that they look OK, talk to your provider about symptoms and next steps.”
A little perspective
Of course, no parent wants their child to get COVID, but in the majority of cases, kids experience much milder symptoms of COVID than adults. And while omicron is affecting people of all ages at record numbers, children still make up a very small percentage of people hospitalized.
According to the American Academy of Pediatrics (AAP), of the 24 states reporting (and New York City), 0.1%-1.6% of all their child COVID-19 cases resulted in hospitalization, with COVID-related deaths in children totaling at 0.00%-0.02%.